Oral Surgery
If you are experiencing any signs or symptoms, such as pain or swelling associated with a tooth that has had a root canal, we encourage you to contact our office immediately to schedule an appointment.
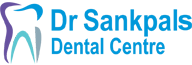
This surgery does not require an overnight stay, and full aftercare instructions and pain medications will be provided as needed. After several days, the dentist will remove the stitches, and the connective tissues will fully heal several months after the procedure.
The dentist will make a small incision in the gum and expose the root by lifting away the gum. In some cases, a tiny fraction of the jawbone may be removed to properly expose the root. The edge of the root tip and any infected connective tissue will be removed using ultrasonic instruments. The root will be sealed using a retrofill (filling material) and the dentist will suture the gum with several stitches.
Prior to the surgery, the dentist will generally prescribe an antibiotic or anti-inflammatory medication to treat the underlying infection. Panoramic x-rays will then be taken to enable the dentist to plan the apicoectomy, which will be performed under local anesthesia.
What does getting an apicoectomy involve?
Narrow or Curved Root Canals. When the root canal is poorly shaped, the endodontic files cannot reach the root tip. Continuing infection or re-infection can then occur. In some cases, the dentist is unable to effectively clean a root canal because it is blocked by a fractured file left behind from prior root canal treatment. Infection and debris can quickly affect adjacent teeth.Small Adjoining Root Branches Roots are extremely complex and can contain many tiny branches. If these tiny branches cannot be cleaned and sealed when the root canal treatment is performed, inflammation can persist.
There are several reasons why an apicoectomy may be necessary
Infected and inflamed soft tissue around the root of a tooth can be exceptionally painful and debilitating to the patient. The purpose of an apicoectomy is to eliminate the infection in the tissue and to ultimately preserve the function of the tooth and save it from extraction. An apicoectomy will rarely be considered by the dentist unless a prior root canal treatment has failed.
Reasons for an apicoectomy
A root canal treatment refers to the cleaning of the canals and the removal of infected and inflamed tissue within the root. When the inflammation or infection persists after the root canal treatment, an apicoectomy may be required. An apicoectomy is essentially the removal of the apex (or root tip), followed by a filling procedure to seal the root from further infection. When left untreated, infected roots can damage other teeth, spread infection, and cause regression of the jawbone.The teeth are held firmly in place by strong roots that extend into the jawbone. Molars and premolars tend to have several roots, whereas the front incisors only have a single root. The end or tip of each root is termed the apex. The apex is where the nerves and blood vessels enter the tooth, and aids in the delivery of blood to the crown (the part of the tooth you can see in your mouth).
Periodontal disease is the leading cause of bone loss in the oral cavity, though there are others such as ill-fitting dentures and facial trauma. The bone grafting procedure is an excellent way to replace lost bone tissue and encourage natural bone growth. Bone grafting is a versatile and predictable procedure which fulfills a wide variety of functions.A bone graft may be required to create a stable base for dental implant placement, to halt the progression of gum disease or to make the smile appear more aesthetically pleasing.There are several types of dental bone grafts. The following are the most common:
Autogenous bone graft In this type of graft the bone is removed from elsewhere in the body and implanted in the mouth. Common donor sites for bone grafting include the iliac section of the pelvis, the chin and the posterior third molar areas of the jaw. If large amounts of bone need to be harvested, the hip or the shin bone (tibia) is generally used.
Allograft Synthetic bone (man made) can be created in the laboratory and used in the bone grafting procedure. Bone can also be obtained from a bone bank (cadaver bone).
Xenograft This is the implantation of bovine (cow) bone. A xenograft is perfectly safe and has been used successfully for many years. Ample bone can be obtained and no secondary donor site is necessary.

Reasons for bone grafting
There are a wide variety of reasons why bone grafting may be the best option for restoring the jaw bone.
Dental implants Implants are the preferred replacement method for missing teeth because they restore full functionality to the mouth; however, implants need to be firmly anchored to the jawbone to be effective. If the jawbone lacks the necessary quality or quantity of bone, bone grafting can strengthen and thicken the implant site.
Sinus lift A sinus lift entails elevating the sinus membrane and grafting bone onto the sinus floor so that implants can be securely placed.
Ridge augmentation Ridges in the bone can occur due to trauma, injury, birth defects or severe periodontal disease. The bone graft is used to fill in the ridge and make the jawbone a uniform shape.
Nerve repositioning - If the inferior alveolar nerve requires movement to allow for the placement of implants, a bone grafting procedure may be required. The inferior alveolar nerve allowsfeeling and sensation in the lower chin and lip.
What does bone grafting treatment involve?
Bone grafting is a fairly simple procedure which may be performed under local anesthetic; however if large amounts of bone area need to be grafted, general anesthetic may be required.Initially, the grafting material needs to either be harvested or prepared for insertion. A small incision is made in the gum tissue and then gently separated from the bone. The bone grafting material is then placed at the affected site.The bone regeneration process may be aided by:
Gum/bone tissue regeneration A thin barrier (membrane) is placed below the gum line over the grafting material. This barrier creates enough space for healthy tissue to grow and separates the faster growing gum tissue from the slower growing fibers. This means that bone cells can migrate to the protected area and grow naturally.
Tissue stimulating proteins Enamel matrix proteins occur during natural tooth development. Emdogain is a matrix protein product which is usually placed on the affected site before the gum is sutured. It mediates the formation of accellular cementum on the tooth which provides a foundation to allow periodontal attachment to occur. Tissue stimulating proteins help to create lost support in areas affected by periodontal defects.
Platelet-rich growth factors A high platelet concentration liquid can be used to create a blood clot at the site of a wound. It has recently been discovered that PRGF also stimulates bone growth meaning a denser graft in a shorter time period.
The gum is sutured in place and a follow up appointment will need to be made within 10 days to assess progress. Bone grafting is a highly successful treatment and a good base for further periodontal restorations.
Reasons for cleft lip and cleft palate correction
Cleft lip and cleft palate are highly treatable deformities, though it may take a whole team of different specialists to fully treat the condition. The prognosis for sufferers who receive corrective treatment is excellent; medically, physically, dentally, and emotionally. There are however, a series of risks for those who do not receive corrective treatment:
- Speech Children born with either cleft deformity are likely to experience speech problems unless treatment is sought. Speech problems are detrimental to a child's social and emotional development.
- Feeding Babies with a cleft palate or a complete cleft lip have problems drinking milk. The gap means that liquids can pass from the mouth to the nasal cavity. This can be dangerous unless the child is fed sitting upright.
- Hearing Loss & Frequent Ear Infections A cleft palate can cause the eustachian tubes (connecting the throat to the ear) to be incorrectly positioned. The fluid build up which results from this poor positioning can lead to painful middle ear infections. Severe and prolonged ear infections can lead to complete hearing loss.
- Dental Issues Abnormalities in the upper jaw, gum, or arch can cause teeth to become impacted (unable to erupt) or absent completely. The shape of the mouth might not permit proper brushing which can lead to periodontal disease and tooth decay.
What does cleft lip and cleft palate treatment involve?
Initially, surgeons will work to close the cleft openings in the first six months of the child's life. Unfortunately, this does not cure the dental problems that occur as a result of cleft lip and cleft palate defects. The dentist will perform a thorough examination of the teeth surrounding the deformity. Panoramic x-rays will generally be taken to allow the dentist to determine the best course of treatment.
The dentist may implant teeth to fill resulting gaps, and/or place braces on the teeth in order to correctly align the upper arch. These treatments will restore functionality to the jaw and improve the aesthetic appearance of the smile. Dental restoration work can generally be performed under local anesthetic and will not require an overnight stay.
If your child was born with any cleft deformity, we strongly encourage you to contact our office to schedule a consultation.
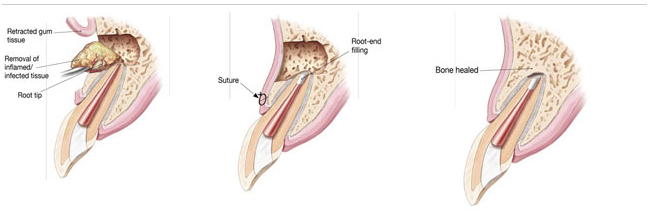
Orthognathic surgery refers to the surgical correction needed to fix substantial abnormalities of the maxilla (upper jaw), the mandible (lower jaw), or both. The abnormality may be a birth defect, a growth defect, or the result of traumatic injuries to the jaw area.
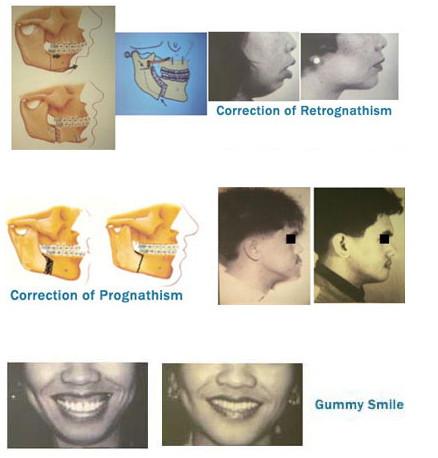
Orthognathic surgery is generally performed by an Oral and Maxillofacial Surgeon to correct malocclusion (bad bite) in cases where routine orthodontic treatment has not or will not be effective. Orthognathic surgeries include the reconstruction of the mandible or maxilla, mandibular ramus, maxilla osteotomy, and mandibular osteotomy.
There are several classifications of malocclusion (the improper coming together of teeth) which may require orthognathic surgery:
Class I Occlusion This malocclusion means that the lower anterior incisors sit directly behind the upper anterior incisors when the patient bites down. This is considered less destructive than Class II and Class III malocclusions.
Class II Malocclusion This is identified when the lower anterior incisors lie significantly behind the upper anterior incisors during the biting process; in some cases hitting the soft tissue behind the upper incisors. This is commonly referred to as an overbite and can cause discomfort, bone damage, excessive wear of the front teeth, and tooth loss.
Class III Malocclusion This is commonly known as an underbite and occurs when the lower anterior incisors and lower jaw are positioned beyond the upper teeth, making the lower jaw much more prominent than the upper jaw.
Reasons for orthognathic surgery
The malocclusion of the teeth can create greatly destructive forces among the five powerful muscles that control the closing and opening of the jaw. These muscles generate a tremendous force when clenching, grinding or chewing. Misalignment can seriously damage the function and aesthetic appearance of the teeth in many ways if left untreated, such as:
- Tooth Wear In the case of an overbite, the pressure and wear on the teeth is not spread evenly. This can also lead to TMJ, migraine headaches, and tooth loss.
- Chronic Jaw, Muscle Pain & Headache The misalignment of the teeth alters the way the facial muscles interact. In some cases, the meniscus cartilage which acts as a buffer between the jawbones can be painfully damaged.
- Loose Teeth When uneven pressure is continually exerted in unintended places or soft tissue is damaged by an overbite, adjacent teeth may become loose in their sockets which causes pain and reduces proper function.
- Tooth Sensitivity As teeth become damaged by constant use, the enamel becomes thinner and the nerves are less protected. This lack of protection can lead to sharp pains when hot or cold foods are eaten.
- Difficulty Swallowing, Chewing, or Biting Food Each can be associated with muscle pain and/or poor alignment of the upper and lower jaws.
What does orthognathic surgery involve?
When the dentist identifies a patient as a candidate for orthognathic surgery, a complete photographic analysis is initially undertaken. This includes panorex x-rays, cephalometric x-rays, models, impressions, and radiographs. Your oral & maxillofacial surgeon, your orthodontist and your dentist will work together and consider how the corrective surgery will impact both proper jaw function and the aesthetic appearance of the entire face.
Generally, orthodontic braces are necessary to align the arches and straighten the teeth prior to the surgery, and additionally, retainers may be used after the surgery. During maxillary surgery, the upper jaw is moved and may be secured in position using tiny plates, wires, rubber bands and screws. Surgery on the mandible is performed using bone grafts to align the lower jaw into the correct position. Orthognathic surgery generally requires a general anesthesia and a good deal of aftercare. Pain medication will be prescribed as necessary, and you'll be given post treatment advice for your recovery. You may also be provided with a modified diet (if required).
Oral & Maxillofacial Surgeons are specialist trained to manage and treat facial trauma. There are an infinite number of ways in which the face can be damaged and thus need some type of reconstruction. Accidents, falls, automobile crashes and interpersonal violence are among the most common causes. Some of the main types of facial injuries resulting from these instances are lacerations, fractured teeth, fractured jaws, fractured facial bones, knocked out teeth and intraoral lacerations.
There are three main classifications used by health professionals in their trauma assessment:
Soft Tissue Injuries Soft tissue trauma includes lacerations to the skin and any kind of intraoral (gum) damage.
Avulsed (knocked out) Teeth - Injuries to the teeth are very common and must be dealt with immediately to insure success of reimplantation.
Bony Injuries This category encompasses the entire face including fractured cheekbones, jaw bones, eye sockets, palates and noses.
Special Regions Special regions refers to the nerves in the face, the eyes, and the salivary glands.
Reasons for Facial Trauma Reconstruction
Aside from the obvious aesthetic reasons for repairing damage to the face, there are also a number of serious health and dental concerns that can arise from even a small amount of trauma. No facial injury should be taken lightly. Depending on the exact location of the injury, respiration, speech and swallowing can be greatly impaired.
Though broken facial bones are generally treated in the emergency room, damage to the teeth can be quickly dealt with by the dentist. Failure to treat dental and facial trauma can lead to the following longer term problems:
- Loss of Functionality: When teeth have fallen victim to trauma, they may become loose in their sockets and make eating and speaking much more difficult.
- Smile Aesthetics: Chipped, broken or missing teeth can be detrimental to a beautiful smile. The dentist is able to repair chips, fractures and missing teeth easily.
- Bite/Jaw Irregularities: After trauma, it is possible that the teeth will become badly aligned. The poor alignment of the teeth can lead to TMJ, uneven teeth wear and other complications.
What does correcting facial trauma involve?
If facial bones have been fractured or broken, they will be treated in much the same way as any other broken bone. Of course, a plaster cast cannot be applied to a cheekbone, but the bones can be held firmly together by either wiring or the insertion of small plates and screws. Soft tissue lacerations will be treated immediately by way of suture (stitching).
In cases where a tooth has been knocked cleanly out of the mouth, there is still a possibility of reinserting it. The quicker a re-insertion can be performed by the dentist, the greater the likelihood that the natural tooth will survive. In the event that the tooth lacks the ligaments necessary for reinsertion, the dentist can implant a prosthetic tooth to restore both functionality and aesthetic appearance. The dentist can also "splint" displaced teeth using structural support such as bonding or wiring with a good amount of success. Root canal therapy is also a possibility for loose or broken teeth.
Your dentist will conduct a thorough examination and take various x-rays in order to determine the precise condition of the afflicted area and plan a course of action. Pain medication will be prescribed as necessary, and you'll be given post treatment advice for your recovery.
Platelet Rich Plasma or PRP is a by-product of blood that is exceptionally rich in platelets. PRP has long been used in hospitals to accelerate the body's own healing process, but it is only fairly recently that advances in technology have allowed this same technique to be used in the dental office.
The blood platelets perform several essential functions in the body, including blood clot formation and the release of growth factors that help to heal wounds. These growth factors stimulate the stem cells to produce new host tissue as quickly as possible, which is why platelet rich plasma is so effective in the post-treatment healing process.
There are several ways in which PRP can be used in clinical dentistry:
Bone Grafting For Implants This includes closure of a cleft lip and cleft palate deformities, sinus lifts, ridge augmentation, and both inlay and onlay grafts.
Bone Repair PRP can be used in facial trauma reconstruction, repairing of defects due to tooth removal, or the removal of growths and cysts.
Fistula Repair This includes the repair of fistulas between the mouth and the sinus cavity.
Reasons for platelet rich plasma treatment
Platelet rich plasma application is now widely used to expedite the post-procedure healing process and is completely safe. Since the blood used will come from the patient's own body, disease transmission is not a factor. Almost all patients report a much greater degree of comfort immediately after their procedure. There are also several more distinct advantages of PRP:
Lower Infection Risk PRP is smeared thickly on the wound after the procedure by the dentist and actually seals the wound away from infectious agents, lowering the risk of problems.
Accelerated Healing The saturation of the wound with PRP helps increase tissue synthesis due to its growth factors, and this in turn results in faster tissue regeneration. Speedier healing decreases the risk of later infections, complications, and discomfort.
Safety and Convenience Disease transmission is non-issue since the blood is harvested from the patient's own blood supply. The amount of blood needed is small and can be collected during a routine outpatient procedure.
What does platelet rich plasma treatment involve?
The dentist will initially assess if your candidate for PRP treatment. Patients with blood clotting disorders will be unable to take advantage of this treatment. A small (about 2 oz) sample of your blood will be collected during a scheduled outpatient treatment. The blood will be placed into a centrifuge to separate the plasma from the red blood cells. A second centrifuge will be used to concentrate the platelets which contain the growth factor.
Immediately after suturing the wound, the dentist will apply the PRP to the surgical area in a high concentration. This will expedite your healing and decrease the amount of discomfort following the surgery. The dentist will provide aftercare instructions pertaining to the surgery and a prescription for pain medication as required.
If you have any questions about treatment with platelet rich plasma or would like to find out if you are a candidate and can benefit from this treatment, please contact our office today to schedule an appointment.
Sleep apnea is a potentially life-threatening sleep disorder characterized by repeated pauses in breathing during sleep. The term sleep apnea is derived from the Greek etymology meaning "without breath". Breathing pauses can last anywhere from several seconds to minutes, and happen as often as 30 times or more per hour. Ongoing disrupted breathing causes an imbalance between the carbon dioxide and oxygen levels in the bloodstream, as not enough carbon dioxide is exiting and not enough oxygen is entering the body.
Sensing this imbalance, the brain sends a message to the body, telling it to wake up to restart breathing the process. People with sleep apnea will partially awake as they struggle to breathe, and this is often accompanied by loud snoring or choking sensations. Because people with sleep apnea don't always completely awake during the episodes, they are often unaware they have a sleeping disorder and it can remain undiagnosed.
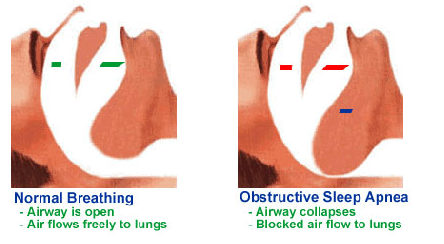
There are two main types of this disorder; central sleep apnea which occurs when the brain fails to send important signals to the breathing muscles, and obstructive sleep apnea which occurs when air cannot flow through the nose or mouth even though the body is still trying to breathe. Obstructive sleep apnea is far more prevalent and easily treatable by the dentist.
Common signs of obstructive sleep apnea can include severe early morning headaches, sleepiness in the daytime, and insomnia. Fortunately, the dentist is equipped with the necessary technology and expertise to treat sleep apnea in several different ways.
Reason for treating sleep apnea
It is very important to seek medical attention if sleep apnea is suspected. A sufferer can completely stop numerous times per hour, and this can quickly turn into a deadly situation. Obstructive sleep apnea occurs when the soft tissue lying at the back of the patient's throat collapses into the airway. The tongue then falls towards the back of the throat which tightens the blockage and prevents oxygen from entering the lungs.
The problem worsens when the chest region, diaphragm, and abdomen fight for air. The efforts they make to obtain vital oxygen only cause a further tightening of the blockage. The patient must arouse from deep sleep to tense the tongue and remove the soft tissue from the airway.
Because sleep apnea causes carbon dioxide levels to skyrocket in the blood and oxygen levels to decrease, the heart has to pump harder and faster to compensate for the lack of oxygen. Sleep apnea patients can technically "die" many times each night. Sleep apnea has been linked to a series of serious heart-related conditions, and should be investigated by the dentist at the earliest opportunity.
What does sleep apnea treatment involve?
Initially, the dentist will want to conduct tests in order to investigate, diagnose, and pinpoint a suitable treatment. The dentist can offer many different treatment options which depend largely on the exact diagnosis and the health of the patient. The dentist may advise the patient to halt some habits that aggravate sleep apnea such as smoking, alcohol consumption, and tranquilizer use.
Sleeping masks were traditionally used to keep the patient's airways open while they slept, but nowadays there are some less intrusive options. Dental devices that gently tease the lower jaw forward are very effective in preventing the tongue from blocking the main air passage. These dental devices are gentle, easy to wear, and often help patients avoid unwanted surgeries.
A more permanent solution is to have surgery that sections the lower jaw and helps pull the bone holding the tongue forward slightly. This surgery has an impressive success rate and is simple for the dentist or oral surgeon to perform. The dentist needs to formally make a diagnosis of each individual case before recommending the best course of action
Tempro-Mandibular Joint Dysfunction Syndrome (TMJ) is a common condition affecting a wide variety of people. TMJ is characterized by severe headaches, jaw pain of varying degrees, grinding teeth, and an intermittent ringing in the ears. The vast majority of TMJ sufferers are unaware that the root cause of these problems is something that a dentist can effectively treat.
The symptoms of TMJ are debilitating and can greatly interfere with every day life. The comfort and general well being of the patient is at the heart of the dental practice, so pain relief is the first consideration of the dentist. The dentist is able to test, diagnose, and devise an immediate plan to treat the underlying causes of the TMJ disorder.
Reasons for treating TMJ
TMJ sufferers report that their symptoms generally worsen during periods of prolonged or unexpected stress, and that intense outbreaks of the condition can lead to neck pain and dizziness.
The most common cause of TMJ is the misalignment of the teeth, often called "bad bite." It is possible for the dentist to realign or adjust the teeth without the need for painful or expensive surgeries. The realignment/adjustment will stop the pounding headaches, the jaw pain, and the dizziness.
The grinding teeth symptom is particularly common and usually occurs at night. The grinding will eventually erode the structure of the teeth and lead to much more severe dental problems in the future. Untreated TMJ is one of the prime underlying factors in eroded jawbones and loose teeth.
It is important for anyone experiencing the symptoms of TMJ to visit the dentist for an exact diagnosis.
What does treating TMJ involve?
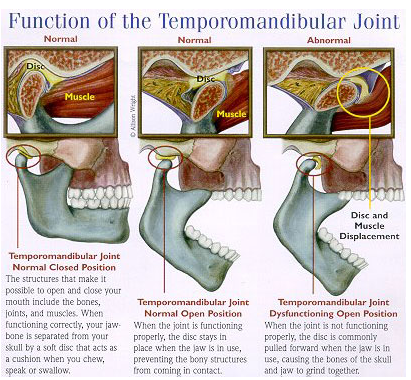
TMJ could be a result of several different problems. Bad bite is the most common, but an injury resulting from a blow to the meniscus cartilage is also a possibility. Initially, the dentist will thoroughly examine the jaw area, the patients bite, take x-rays, and review the patient's history in order to make an accurate diagnosis and recommend necessary treatment.
Once a firm diagnosis is attained, there are several ways in which relief can be provided. A specially molded bite guard can be created to stop teeth grinding during the night. A bite relationship analysis may be recommended by the dentist. The dentist can also provide advice on relaxation techniques which will lessen the effects of stress. As a last alternative, the dentist is also able to prescribe muscle relaxants.
A better option is to change the shape of the teeth and get rid of the bad bite completely, often called "realignment." This is especially useful because it alleviates TMJ symptoms and may improve the aesthetic appearance of the teeth as well. Realignment involves adjusting the relationship between how the upper teeth come together with the lower teeth. This may require new restorations and/or adjusting the natural teeth as well. It is not a painful procedure, and it is one the dentist has performed with great success numerous times. As with any procedure, the dentist will be happy to answer questions and discuss symptoms, options, and treatments.
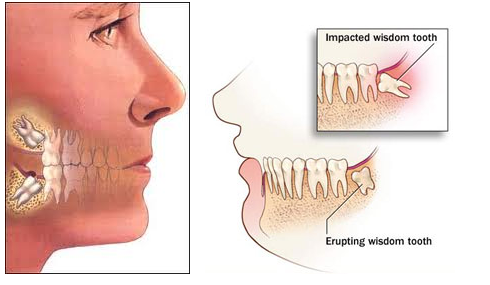
Third molars, commonly referred to as wisdom teeth, are usually the last four of 32 teeth to erupt (surface) in the mouth, generally making their appearance between the ages of 17 to 25. They are located at the back of the mouth (top and bottom), near the entrance to the throat. The term "wisdom" stems from the idea that the molars surface at a time typically associated with increased maturity or "wisdom".
In most cases, inadequate space in the mouth does not allow the wisdom teeth to erupt properly and become fully functional. When this happens, the tooth can become impacted (stuck) in an undesirable or potentially harmful position. If left untreated, impacted wisdom teeth can contribute to infection, damage to other teeth, and possibly cysts or tumors.
There are several types, or degrees, of impaction based on the actual depth of the teeth within the jaw:
Soft Tissue Impaction: The upper portion of the tooth (the crown) has penetrated through the bone, but the gingiva (gum) is covering part or all of the tooth's crown and has not positioned properly around the tooth. Because it is difficult to keep the area clean, food can become trapped below the gum and cause an infection and/or tooth decay, resulting in pain and swelling.
Partial Bony Impaction: The tooth has partially erupted, but a portion of the crown remains submerged below the gum and surrounding jawbone. Again, because it is difficult to keep the area clean, infection will commonly occur.
Complete Bony Impaction: The tooth is completely encased by jawbone. This will require more complex removal techniques.
Reasons to remove wisdom teeth
While not all wisdom teeth require removal, wisdom teeth extractions are most often performed because of an active problem such as pain, swelling, decay or infection, or as a preventative measure to avoid serious problems in the future. If impaction of one or more wisdom teeth is present, and left untreated, a number of potentially harmful outcomes can occur, including:
Damage to nearby teeth: Second molars (the teeth directly in front of the wisdom teeth) can be adversely affected by impacted wisdom teeth, resulting in tooth decay (cavities), periodontal disease (gum disease) and possible bone loss.
Disease: Although uncommon, cysts and tumors can occur in the areas surrounding impacted wisdom teeth.
Infection: Bacteria and food can become trapped under the gum tissue, resulting in an infection. The infection can cause considerable pain and danger.
Tooth Crowding: It has been theorized that impacted wisdom teeth can put pressure on other teeth and cause them to become misaligned (crowded or twisted). This theory isn't universally accepted by all dental professionals, and it has never been validated by any scientific studies.
Wisdom teeth examination
As with any dental procedure, your dentist will want to initially conduct a thorough examination of the wisdom and surrounding teeth. Panoramic or digital x-rays will be taken in order for your dentist to evaluate the position of the wisdom teeth and determine if a current problem exists, or the likelihood of any potential future problems. The x-rays can also expose additional risk factors, such as deterioration or decay of nearby teeth. Early evaluation and treatment (typically in the mid-teen years) is recommended in order to identify potential problems and to improve the results for patients requiring wisdom teeth extractions. Only after a thorough examination can your dentist provide you with the best options for your particular case.
What does the removal of wisdom teeth involve?
Wisdom teeth removal is a common procedure, generally performed under local anesthesia, intravenous (IV) sedation, or general anesthesia by a specially trained dentist in an office surgery suite. The surgery does not require an overnight stay, and you will be released with post-operative instructions and medication (if necessary), to help manage any swelling or discomfort.